Digestive System
Digestive System
Our Gastroenterology Unit, led by Dr. López Cano, a specialist in Digestive System with training in Spain, Italy, and the United States, comprises a team of 6 specialists who handle over 30,000 cases annually and perform around 6,000 endoscopic procedures each year.
Diagnosis and treatment of digestive system diseases
General ultrasound diagnosis; doppler ultrasound and interventional ultrasound
Endoscopic, ecoendoscopic and endoscopic capsule diagnosis.
The Team
Our specialists have received training from prestigious medical centers such as the Mayo Clinic in New York, the University Hospital of San Diego (California), and the Clinical Hospital of Barcelona. Some have held leadership positions in important scientific societies, such as the Spanish Society of Digestive Ultrasonography, and are members of others, including the Spanish Society of Digestive Endoscopy, the Spanish Society for the Study of the Liver, and the National Group of Ecoendoscopy.
Our unique focus on the prevention, diagnosis, and treatment of digestive pathologies attracts a significant percentage of patients from relatively distant areas of Cádiz seeking definitive solutions to their problems.
Our collaboration with centers like the Reina Sofía Hospital in Córdoba and the University Clinic of Navarra is constant and fluid.
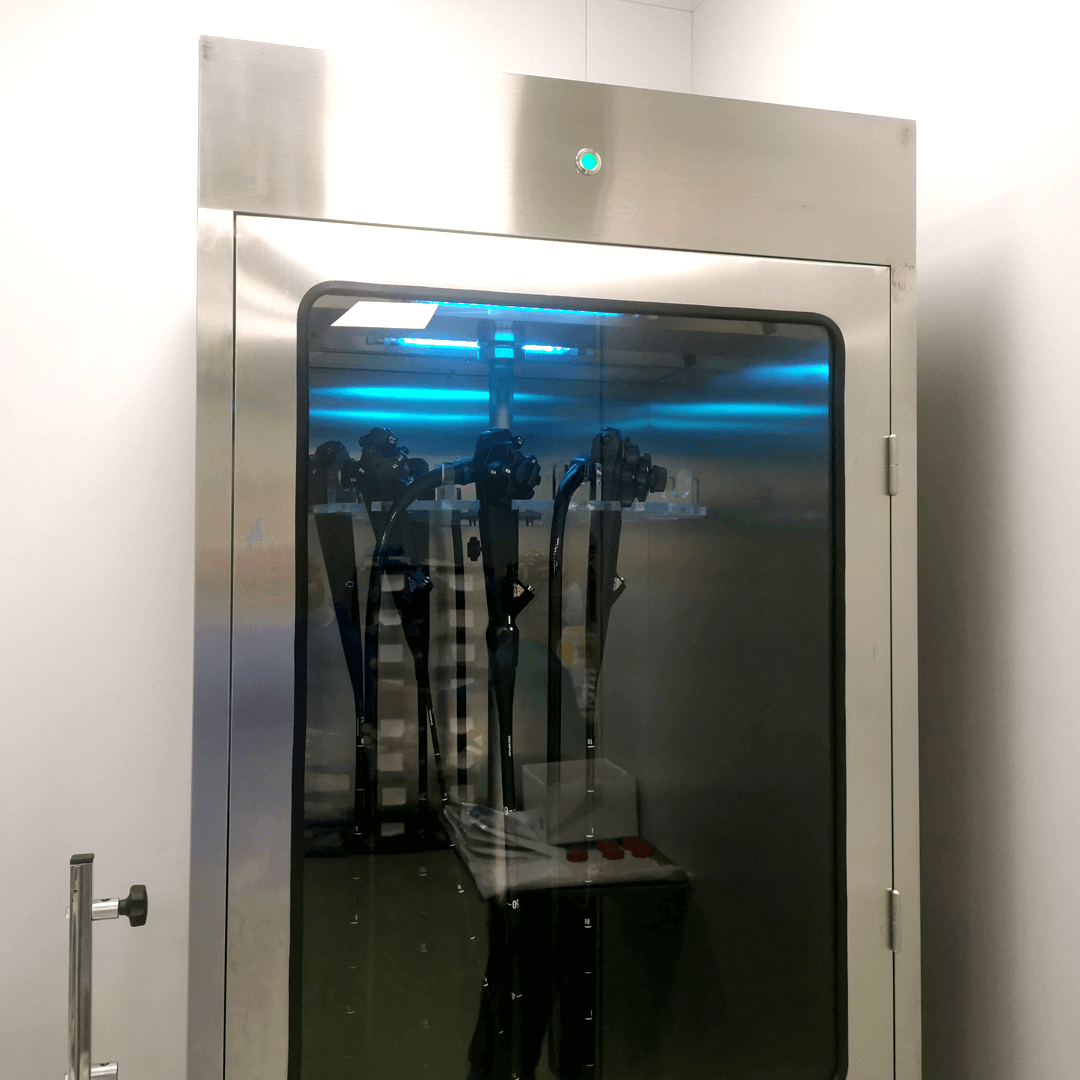
Innovation and advanced technology at the service of your health
Techniques
Capsule endoscopy
A non-invasive diagnostic technique involving the use of a small video camera, swallowed like a pill, to capture images of the small intestine.
Urease breath test
A comfortable and straightforward test that analyzes the air we exhale to detect the ‘Helicobacter pylori’ bacteria in the stomach, responsible for various gastric and duodenal ailments.
Esophageal Manometry
Measures pressure and muscle contraction patterns in the esophagus. Abnormalities in these parameters can lead to pain, acidity, and swallowing difficulties. The procedure involves inserting a thin tube into the esophagus through the nose.
Anorectal manometry
Lactose intolerance can be due to a reduced production of the enzyme lactase in the intestine, resulting in symptoms such as gas, abdominal bloating, and occasional diarrhea. This test involves exhaling air, in which we measure the amount of hydrogen, which is related to the deficiency of the enzyme.
pH Monitoring
An essential exploration for studying gastroesophageal reflux disease, characterized by heartburn and acid regurgitation. pH monitoring, performed using a small tube inserted through the nose, identifies over 95% of patients with reflux and assesses its severity.
Abdominal ultrasound
A harmless technique using ultrasound to visualize internal organs in the abdomen, such as the liver, gallbladder, spleen, pancreas, kidneys, bladder, prostate, and peritoneal and retroperitoneal spaces. Blood vessels (inferior vena cava, aorta, etc.) can also be examined.
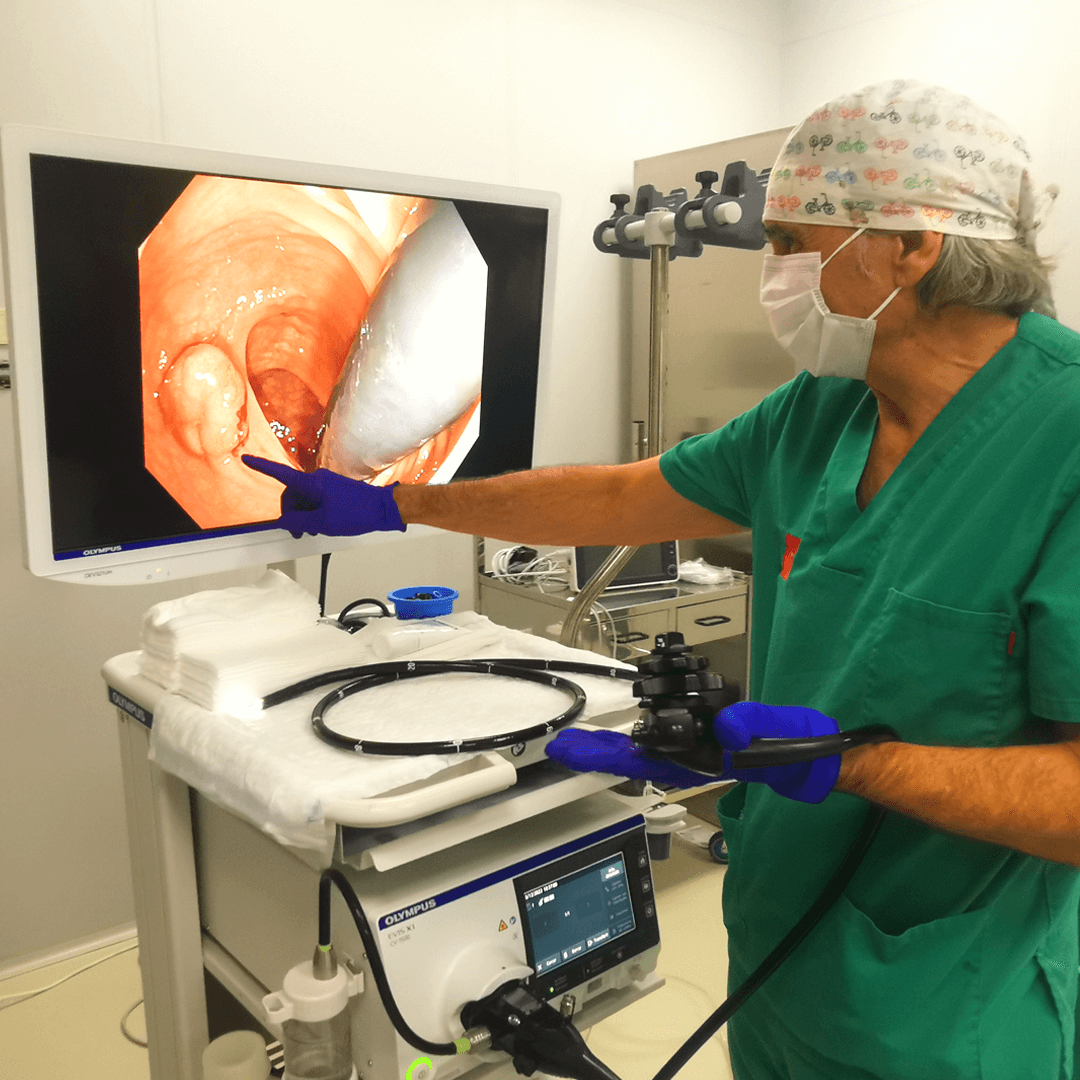
Diagnostic Upper and Lower Endoscopy
These explorations involve flexible tubes inserted through the mouth or anus, equipped with a camera to visualize the interior of the digestive tract. Upper endoscopy examines the esophagus, stomach, and duodenum, while lower endoscopy allows examination of the entire colon and even the last centimeters of the small intestine. Both procedures allow for biopsies and certain therapeutic interventions and are performed under sedation.
Therapeutic endoscopy
A set of techniques guided by endoscopes that allow the cure of certain lesions or palliation of others to improve the patient’s quality of life and prognosis (removal of polyps, tumors, or placement of prostheses). Most of these techniques are performed on an outpatient basis and under sedation.
High and low echo-endoscopy
An exploration that allows for the direct visualization of the inside of the upper intestine, rectum, and sigmoid, as well as the surrounding structures (mediastinum, pancreatic region, biliary tract, pelvic cavity). The ecoendoscope, a tubular endoscope with an incorporated ultrasound probe, provides both endoscopic and ultrasound views of the entire environment and is performed under sedation.
Ecoendoscopy with Puncture
Using an ecoendoscope and a special needle, this technique allows for the collection of material to be studied under a microscope, helping diagnose tumors and other lesions accurately.
Elastography / FibroScan
A technique performed with a probe similar to an ultrasound, used to study liver diseases. It is non-invasive, simple, and quick, improving the diagnosis and monitoring of liver fibrosis without the need for a biopsy. It has no side effects or risks for the patient.
Diagnostic and therapeutic interventional ultrasound
Ultrasound offers significant advantages as a guide for procedures, as it is mobile, does not use ionizing radiation, and requires less time than other techniques. The procedures involve inserting a needle or catheter through the ultrasound’s imaging plane. The advancement is controlled in real-time, allowing precise targeting of the area for diagnosis or treatment. Common procedures include biopsies, drainage, and percutaneous injections.
Abdominal Ecodoppler
A type of ultrasound used to study the flow of blood through arteries and veins, providing information about their quantity and velocity. It is very useful for studying portal hypertension, abdominal tumors, and inflammatory bowel disease, among other pathologies.
Contrast Ultrasound (Sonovue)
Used to enhance ultrasound images by increasing the vascular signal in arteries and veins. It is particularly employed in characterizing abdominal tumors and diagnosing Crohn’s disease. Contrast is injected through a vein in the arm, and within seconds, it reaches the abdominal vessels, which can then be visualized with ultrasound. The contrast is eliminated through breathing.
Make an appointment
Request your first free appointment






